Why I Hope to Be Alive at 75 – Article by Steve Hill

Steve Hill
Editor’s Note: In this article, originally published on November 13, 2020, by our allies at the Life Extension Advocacy Foundation (LEAF), Steve Hill explains why the attitude of Joe Biden’s new advisor on COVID-19 strategy, Ezekiel Emanuel, is supremely counterproductive. Emanuel infamously wrote in 2014 that he hopes to die at age 75. Given that COVID-19 is a disease whose toll is greatly amplified by biological aging, Emanuel’s statements render him uniquely ill-suited to remedy the ravages of the ongoing pandemic. Moreover, his pessimism toward what life is like at age 75 is no longer justified, in light of emerging medical advances that could enable rejuvenation and biological youthfulness for those who are in late middle age today. Perhaps, if he sees these advances become a reality in the not-too-distant future, Emanuel might change his mind regarding the desirability of longer lifespans.
~ Gennady Stolyarov II, Chairman, United States Transhumanist Party, November 17, 2020
2020 has been a strange year for a variety of reasons, but the societal changes that the COVID-19 pandemic has created are probably the strangest. However, it is perhaps even stranger that Dr. Ezekiel Emanuel has been appointed to advise Joe Biden on COVID strategy.
Emanuel is best known for writing a controversial article in the October 2014 edition of The Atlantic, headlined “Why I Hope to Die at 75”, in which he strongly rejects the desire to live beyond the age of 75 and expresses his opinion that continuing to live after such an age is meaningless.
Living too long is also a loss. It renders many of us, if not disabled, then faltering and declining, a state that may not be worse than death but is nonetheless deprived.
Needless to say, I strongly disagree with this baffling point of view and am somewhat concerned that someone who thinks this way of his own life, and presumably the lives of others, may be appointed to a position of influence for a disease whose primary risk group is the elderly. This seems almost as foolhardy as spending a vacation weekend in a caravan with Hannibal Lecter.
Emanuel listed quite a few methods by which people extend their lives and stated that they were a “valiant effort to cheat death and prolong life as long as possible,” but his response to them was, “I reject this aspiration. I think this manic desperation to endlessly extend life is misguided and potentially destructive.”
Age is the #1 risk factor for COVID
The scientific evidence clearly shows that the primary risk factor for contracting and dying from COVID-19 is age, with people over the age of 75 at particularly high risk. This is due to the decline of the immune system, which becomes increasingly weak and dysfunctional with age in a process known as immunosenescence.
Globally, the strategy has been to try to shield these vulnerable people as best as possible due to their weakened immune systems and limit their exposure to the disease while vaccines are developed.
Needless to say, I find Biden’s nomination of him to address a disease that mostly affects seniors ironic in itself, given that he thinks the lives of most people beyond 75 are pointless and that they don’t live meaningful lives and would be better off embracing death rather than desperately trying to extend them. Therefore, I hope for the sake of the older people in our society that he has rethought his priorities.
Why I hope to be alive at 75
Predictably, there is already a storm raging on social media around his appointment, so there is no purpose to adding more fuel to that fire. Instead, I am going to talk about why the future of aging could be very different to the grim picture that Emanuel paints.
At age 63, he is getting closer to the age at which he thinks life is pointless, and I believe that a large reason why he is so pessimistic about life beyond 75, whether he realizes it or not, is based on the current state of medicine. This line of reasoning does not take into account how medicine, and in particular how we treat aging could change in the next decade or two.
Current medicine does a great job at keeping people alive for longer, but they often have to live with one or more chronic diseases. Given that, I am not surprised that Emanuel is not enamored with living a long life, especially as that could entail being disabled, bed-bound, or otherwise suffering a poor quality of life as the result of debilitating age-related diseases.
Thankfully, the world healthcare strategy is slowly starting to shift to one of prevention over cure, but right now, the typical approach is to play whack-a-mole with diseases. As one pops up, it is treated, then the next, and the next, and so on. This strategy works great for infectious diseases, but it is an exercise in futility and diminishing returns when applied to the chronic diseases of aging.
However, things could be different in the not so distant future, and being 75 could see the majority of people far more fit, healthy, and vibrant than ever before in human history thanks to advances in aging research. Therapies that directly target aging could potentially make people biologically younger (in particular their immune systems) and much more able to withstand COVID-19 and other diseases.
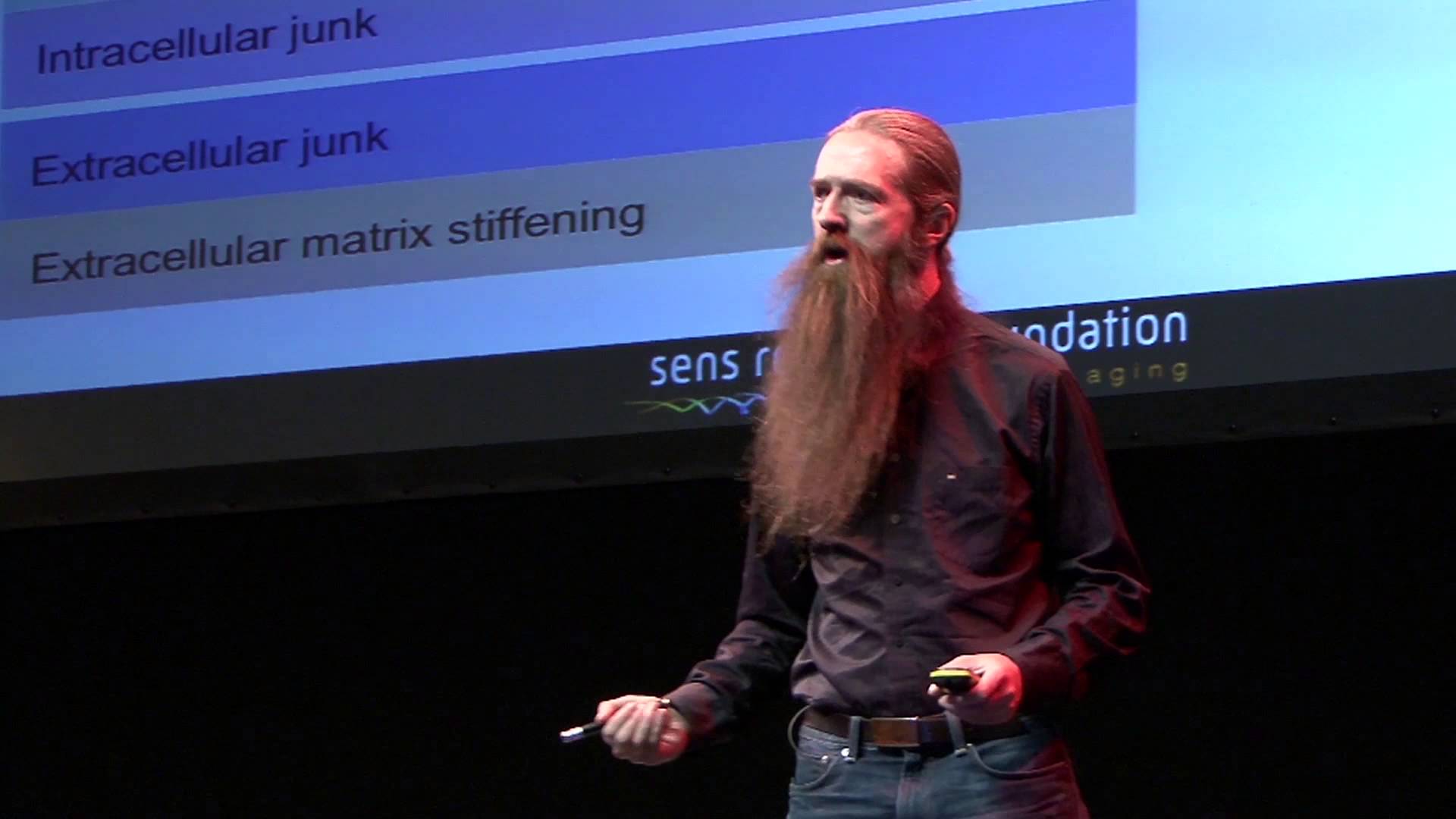
As explained on LEAF’s What is Aging? page, aging consists of multiple processes (“hallmarks”) that gradually cause damage to organs and tissues and lead to age-related diseases. Rejuvenation biotechnology is advanced medical technology that directly addresses any of the various aging processes in order to restore tissue and organ function to a more youthful state, thereby ameliorating, delaying, or preventing age-related diseases. Let’s take a brief look at some of the promising near-future research that could bear fruit by the time Emanuel reaches 75 and perhaps change his mind.
Rejuvenating the immune system
The decline of the immune system is a key reason why the elderly are most susceptible to infectious diseases such as COVID, and there has been considerable interest in the rejuvenation of the immune system in recent years.
Dr. Greg Fahy from intervene immune has had some early success with thymus rejuvenation in a small human pilot study and demonstrated that it is possible to cause the thymus, which shrinks and loses its capacity to produce immune T cells during aging, to regrow and resume production of those cells. Dr. Fahy is now moving forward into a larger-scale study, and if the results continue to be positive, it is not hard to imagine that thymus regrowth could become a staple of helping the elderly stay healthy.
Another example of immune rejuvenation is currently being developed by Samumed, a biotechnology company that is developing drugs that target the Wnt pathway to restore it to youthful function. The Wnt pathway is a key pathway that regulates the function of our stem cells and ensures that they supply our tissues and organs with new cells to replace losses from injury, disease, and wear and tear.
If successful, this approach would allow the body to resume efficient repair of tissues, and it would replenish aged and failing tissues and organs with fresh, healthy cells supplied by the rejuvenated stem cells.
Therapeutic plasma exchange
Researchers Irina and Mike Conboy at UC Berkeley have been researching blood factors and their role in aging for over two decades. During that time, they have identified a number of factors present in aged blood that appear to regulate aging.
These factors are also present in younger people, but in typically far lower amounts, and tend to serve useful functions. However, during aging, the levels of these proteins become deregulated, and they often rise to detrimental levels and cause damage to the body, which typically involves preventing stem cells from working and tissue from regenerating.
Decades’ worth of research from the Conboy lab has shown that, in mice at least, it is possible to filter out these harmful pro-aging blood factors and bring them back down to a level similar to younger animals. When this happens, the result is rejuvenation of tissues and the reversal of some of the aspects of aging, making the mice more youthful.
This approach uses an already approved technique known as therapeutic plasma exchange to filter and calibrate these key factors and could be readily modified for human use. Should the results seen in animals translate to humans using this approach, it would have a profound effect on our health as we age and potentially delay, prevent, or even reverse some age-related diseases.
Conclusion
These are only some of the examples of why healthy life expectancy could rise significantly in the near future, and there are plenty of reasons to remain future positive. This is the future direction of medicine and healthcare that we support at Lifespan.io, a world where being 75 does not mean you are thrown on the scrap heap and where people like Emanuel will no longer feel that life has no meaning. I am confident that in such a world, being 75 would not be the burden he thinks it will be, and this is why I hope to be alive at 75.
Steve Hill serves on the Life Extension Advocacy Foundation (LEAF) Board of Directors and is the Editor-in-Chief, coordinating the daily news articles and social media content of the organization. He is an active journalist in the aging research and biotechnology field and has to date written over 500 articles on the topic, interviewed over 100 of the leading researchers in the field, hosted livestream events focused on aging, along with attending various medical industry conferences. His work has been featured in H+ Magazine, Psychology Today, Singularity Weblog, Standpoint Magazine, Swiss Monthly, Keep Me Prime, and New Economy Magazine. Steve has a background in project management and administration, which has helped him to build a united team for effective fundraising and content creation, while his additional knowledge of biology and statistical data analysis allows him to carefully assess and coordinate the scientific groups involved in the project.
















 Steve Hill
Steve Hill