U.S. Transhumanist Party Chairman’s Fifth Anniversary Message

Gennady Stolyarov II
Gennady Stolyarov II, Chairman, United States Transhumanist Party
Time advances inexorably, and it has already been five years since I became Chairman of the U.S. Transhumanist Party on November 17, 2016. While my tenure as Chairman began during a politically turbulent time in the United States, I could not have envisioned the extent of volatility, external shocks, social fractiousness, and, frankly, the steady deterioration of civilization and its displacement by sheer mass insanity – all of which have characterized 2021 even more amply than 2020. The COVID-19 pandemic, originally portrayed as a temporary disruption that could be overcome with a bit of collective precaution and shared inconvenience, has stubbornly resurged multiple times despite periodic false dawns – and despite extremely impressive and highly efficacious achievements of science and technology deployed to fight it. The lessons of 2021 are in many regards sobering – but the most significant of them is this: When the world and its major institutions and social norms are steadily disintegrating all around one, there is no choice but to rely on what one can build oneself, in collaboration with other good people who care about emerging into a brighter future.
For me, it has become clearer than ever why the U.S. Transhumanist Party exists and must continue to exist. We are the bulwark against the chaos. Our Core Ideals, our Platform, our vision for the next, greatest era of our civilization, are the inspiration, the fuel needed to propel ourselves as individuals and humankind as a species out of this pandemic and into the type of world that we can achieve and that we deserve. Leading such an organization is an ultramarathon and not a sprint – a distinction with which I am familiar quite literally. This is why my first thought on the occasion of my five-year Chairmanship anniversary, expressed to the USTP members on November 17 of this year, was that staying the course and integrity of vision are crucial!
For those who are interested in my general thoughts about how transhumanism offers a way out of the current predicament and toward a reinvigorated, widespread sense of meaning and impetus toward progress in all areas of society, I recommend watching my presentation “Regaining Civilizational Sanity Through Transhumanism” – originally delivered at the Vanguard Scientific Instruments in Management 2021 (VSIM-2021) conference on September 11, 2021.
We have put forth a valiant effort during the past year to both improve our organization and expand our reach. We now have over 3,700 members, and we continue to grow through our offering of free membership in perpetuity. Our Virtual Enlightenment Salons have been streamed every week without fail; we now have hundreds of hours of content from 82 sessions since the start of the pandemic, which have been compiled into a regularly updated YouTube playlist. The Virtual Enlightenment Salons have, indeed, been a bright light during this pandemic, bringing an interdisciplinary approach toward addressing the most pressing challenges faced by our species and arriving at advanced insights through long-form conversations in ways that would have made the 18th-century Enlightenment philosophers proud. (Of course, the 18th-century Enlightenment philosophers would have wished that they could have had our level of communication technology and means to engage in hours-long conversations with people from all over the world!) Our most-watched conversations during this past year have been our Virtual Enlightenment Salons with Aubrey de Grey and Natasha Vita-More – both pivotal figures in our movement whose influence continues to be profound – and various sessions with other honored guests have come close in terms of viewership as well. We have used the Virtual Enlightenment Salon as a forum to test innovative formats of interaction, such as our Debate on Artificial General Intelligence and Existential Risk between Connor Leahy and David J. Kelley on February 7, 2021, and our Special Panel on FDA Reform on April 4, 2021 – both among our most-attended events. Most recently, the USTP has partnered with KGRA Radio to further improve the production quality of the Virtual Enlightenment Salons and effectively double our audience. Our conversations thus far with David Pearce, FairVote Washington, and Greg Mustreader illustrate the promise of this new format for the hopefully many sessions to come.
Setting for the U.S. Transhumanist Party Virtual Enlightenment Salons – Background by Art Ramon Garcia, Jr., USTP Director of Visual Art
We have also used the Virtual Enlightenment Salon venue for internal organizational improvement, as illustrated prominently during our Reform Summit of November 28-29, 2020, during which we laid the groundwork for improvements to our Constitution which have resulted in significantly greater stability for our organization and strengthened eligibility criteria for endorsing candidates and appointing Officers, which have since been applied with the intended effects. We continue to implement the other reforms discussed at that Summit, including taking incremental steps toward accepting small donations via YouTube Super Chats and merchandise sales (here and here) to pay for website hosting and develop a small budget for future in-person events.
The new candidate vetting process has led to our most successful candidate endorsement yet, as we supported the campaign of Jennifer A. Huse for Mayor of Camden, New Jersey. (See our original candidate interview with Jennifer and our subsequent May 2 and October 17 Virtual Enlightenment Salons with her.) Jennifer ran a determined campaign, gaining inclusion on the general-election ballot through a remarkably persistent petition drive and overcoming dishonest tactics from one of her opponents who sought to have her disqualified based on false allegations. She personally reached out to hundreds of residents of Camden and engaged them directly on the issues that mattered most to them, while earning the distinction of being the first mayoral candidate in the United States to specifically focus on life-extension initiatives within her platform. Ultimately Jennifer received 104 votes in the general election, or 1.61% of the total – overcoming a near-complete lack of media coverage of her campaign to nonetheless reach many voters who were dissatisfied with decades-long mismanagement of Camden by the Democratic Party. (Jennifer’s only other “independent” opponent, Theo Spencer, was in fact a Democrat who chose to run against the incumbent Democratic Mayor and temporarily became an “Independent” to do so.) Just by giving voters an alternative to the Democratic Party monopoly in Camden, Jennifer made a great breakthrough in the politics of that area, as now the Democrats know that they face the possibility of competition if they allow the situation to deteriorate any further. Moreover, Jennifer’s campaign provided key lessons in how transhumanists can run for local office and integrate the ideas of transhumanism with the local issues that matter most to their constituents, providing that crucial connection between the overarching promise of transhumanism and the practical solutions to day-to-day challenges in ways that could lead to immediate quality-of-life improvements for residents.

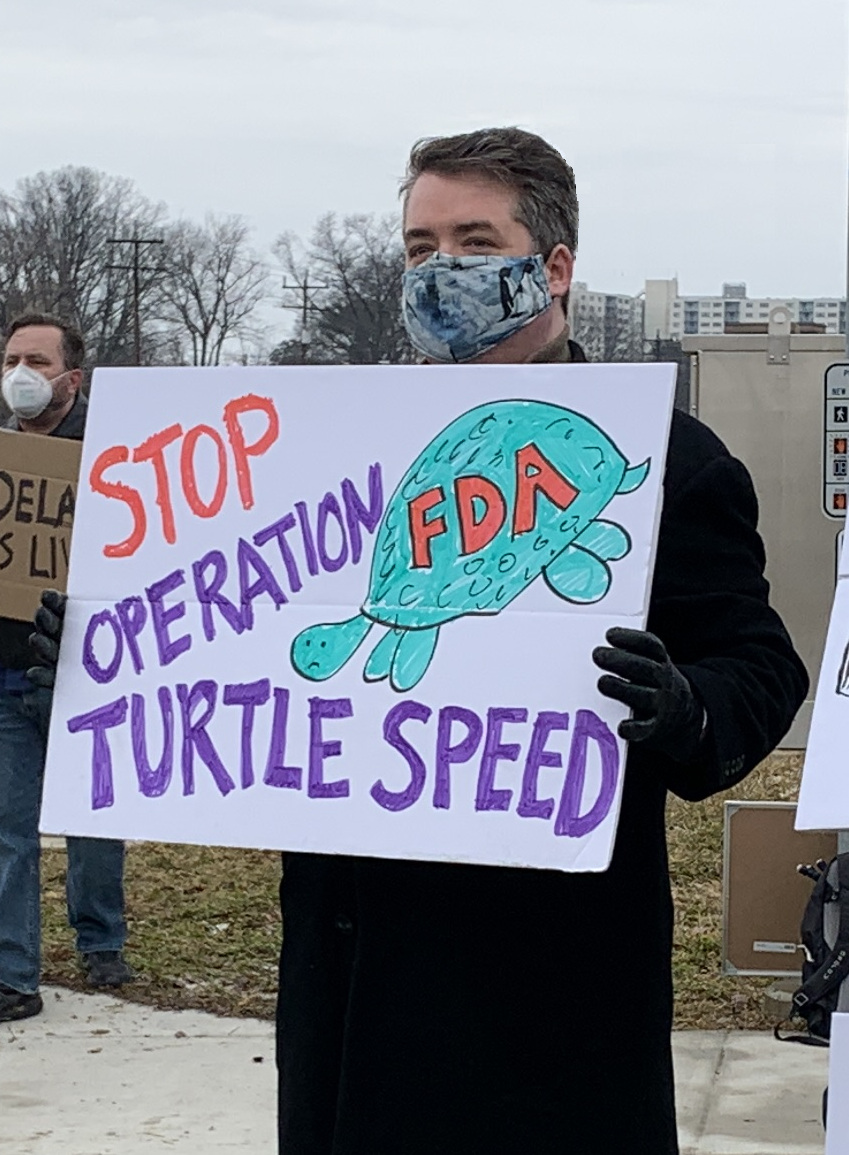
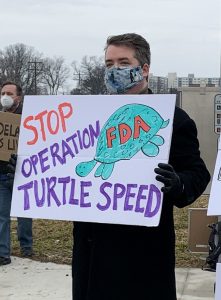
The USTP undertook diligent efforts at political activism earlier in 2021. We were not always successful, but we made our presence known. From protesting near the FDA headquarters in Maryland to urge prompt approval of the Johnson & Johnson and AstraZeneca COVID-19 vaccines (read our Director of Scholarship Dan Elton’s letter to the FDA here), to testifying multiple times in opposition to Nevada Senate Bill 292 (which imposed an onerous “equal distribution” requirement for petition signatures of minor political parties, effectively preventing new minor parties from gaining ballot access), to writing to a Joint Special Committee of the Nevada Legislature in support of the concept of Innovation Zones, we endeavored to make a difference where we could, advocating for policy changes that would have saved lives, accelerated medical progress, prevented additional barriers to political participation, and enabled technological development to flourish. In politics one unfortunately does not get to win every battle, but even bringing a pro-technology, pro-rationality voice into political conversations, in a way that gets noticed by the key decision-makers, is itself a crucial step forward.


“Unclog the FDA” Pro-Vaccine Protests Near the FDA Headquarters in Silver Spring, Maryland – February 14, 2021
Just as 2021 has been highly unpredictable in its greater-than-anticipated turbulence, so does even the near-term future continue to be difficult to anticipate or plan for in any meaningful respect. However, I can identify several broad goals for the upcoming year of my Chairmanship:
1. Establish the Transhuman Club, the apolitical affiliate of the USTP, as a functioning organization.
2. Create a list of ongoing USTP projects to which members can contribute their efforts.
3. Test the approach of focused working groups for several ongoing projects.
4. Resurrect and release LEV: The Game, a computer game illustrating the concept of longevity escape velocity.
5. Hold at least one in-person event (possible provided that the pandemic subsides to a substantial extent).
6. Train the core of volunteers needed to publish content on the USTP website and spread it throughout various social media on a regular basis.
7. Create coordinated teams of USTP members and allies to monitor key online spaces for mentions of transhumanism and key figures in our movement, and to ensure that accurate information is presented and not targeted for deletion and censorship by our intolerant adversaries.
8. Reach 5,000 members. This will be an important milestone, halfway to the 10,000-member threshold which will hopefully enable the organization to become self-sustaining in perpetuity.
9. Continue the weekly Virtual Enlightenment Salons and create a large series of short video excerpts from numerous Salons so as to reach audiences who have tighter time constraints or who are seeking more concise introductions to transhumanist ideas.
10. Continue to strengthen policies and social-media tactics to protect the transhumanist community against trolls and hostile entryists with ulterior motives.
Too many individuals and organizations, when faced by challenges, come to turn inward and to doubt themselves, doubt their mission, doubt the validity of their ideas or the efficaciousness of their approach. Just because they do not get instant results (especially when the actual results may manifest over the course of years and decades), they come to question the ultimate goal – or try to make so many adjustments or “pivots” at once that they really have no objective means of testing whether the changes are genuine improvements or mere expenditures of energy borne out of frustration. Yet when the organization’s ideas and values are sound, when the culture is constructive, when the goals are worthwhile, then the main essential approach is to continue to work consistently and energetically for the fulfillment of those goals. Incremental reform is, of course, feasible and desirable, and there are always ways in which any organization, or any person, can improve. But as the 2009 version of the Transhumanist Declaration wisely points out, “Although all progress is change, not all change is progress.” Organizational reform efforts also need to be diligent about preserving and amplifying what aspects of the organization do work well; they need to be deployed surgically and mindfully to ensure that any given change does, indeed, constitute progress.
Our critics – the techno-pessimists, the partisans of the duopoly, the alt-right conspiracy theorists, the online trolls, the misguided ideologues of zero-sum new social movements – will not hesitate to use every opportunity to point out what they perceive to be our flaws. We must resist the temptation to be cowed by them or to “rebrand” ourselves in reaction to every perceived manifestation of hostility. Make no mistake about it, our movement is under attack from many corners – both from the typical detractors and from those “strategic conservatives” who wish to tone down our messaging for fear that it might rankle mainstream institutional gatekeepers – as well as from sheer unscrupulous opportunists who seek to rise by manufacturing scandal and tearing down prominent figures with long records of accomplishment. Alarmingly, the tactics of those who attack us from both without and within have become increasingly heavy-handed, indiscriminate, and outright dishonest, and certain well-known events of the past several months have illustrated this quite clearly. Yet in the words of Victor Hugo, “You have enemies? Why, it is the story of every man who has done a great deed or created a new idea.” Having the right enemies may, indeed, be a sign that an idea is attracting notice and gaining influence; this is the situation of transhumanism today as the world seeks answers about how we can avoid the repetition of the horrific events of 2020 and 2021 in the years and decades to come. Our most significant challenge is not to concern ourselves with what our critics think of us, but rather to reach the vast majority of people who are still unfamiliar with what transhumanism is and what it stands for, as well as the direct relevance of transhumanist ideas to their lives. Reaching people outside of our immediate circles is no easy task; it requires a significant time commitment and grass-roots, often one-on-one, persuasion and advocacy. Most importantly, this is not an effort that any of us can succeed at alone. Our community, and the USTP as an organization in particular, are absolutely crucial to facilitating an infrastructure and set of shared resources that we can use to reach broader segments of the public and motivate others to add their voices and skill sets to our outreach initiatives.
I continue to firmly believe that we, the human species in general and transhumanists in particular, can emerge from these troubled times together – but only together – only in a spirit of mutual uplifting and perseverance in the face of adversity. As Chairman of the U.S. Transhumanist Party, there is much that I am able to achieve, but I cannot achieve it alone. In the coming months, you, the members of the USTP, will receive more information about how you can assist in our mission in structured, straightforward ways. As I have urged transhumanists and the USTP to stay the course in our fidelity to our values, so I will aim to provide the means for many of you to do so effectively and contribute toward the realization of the transhumanist vision. The near-term future will continue to be ambiguous, perilous, and tragic at times – but I maintain that, slightly beyond the thick fog of the present, a luminous expanse awaits us. Through our own efforts, moving unceasingly forward, we can reach it – and soon.